Report – Rural eMental Health
Aboukarr S, LeBlanc M, Petrie S, Carson DB, Paskaran S, & PA Peters. (2019) Report: Best Practices for Rural eMental Health. Spatial Determinants of Health Lab, Carleton University: Ottawa, ON. DOI:10.22215/sdhlab/2019.2
A high-quality PDF of this report is available for download.
The more “rural” or “remote” a community, access to mental health services decreases. By mitigating barriers and promoting enablers, successful eMental health integration can increase access to mental health services for rural residents.
eMental health aims to bridge the gap between rural and urban mental health services by introducing electronic methods such as teleconferencing or video conferencing for psychological services, virtual referral to psychiatrists, and sharing of electronic records. Successful integration of the technology remains a challenging task, with key actors, enablers, and barriers all influencing its success.
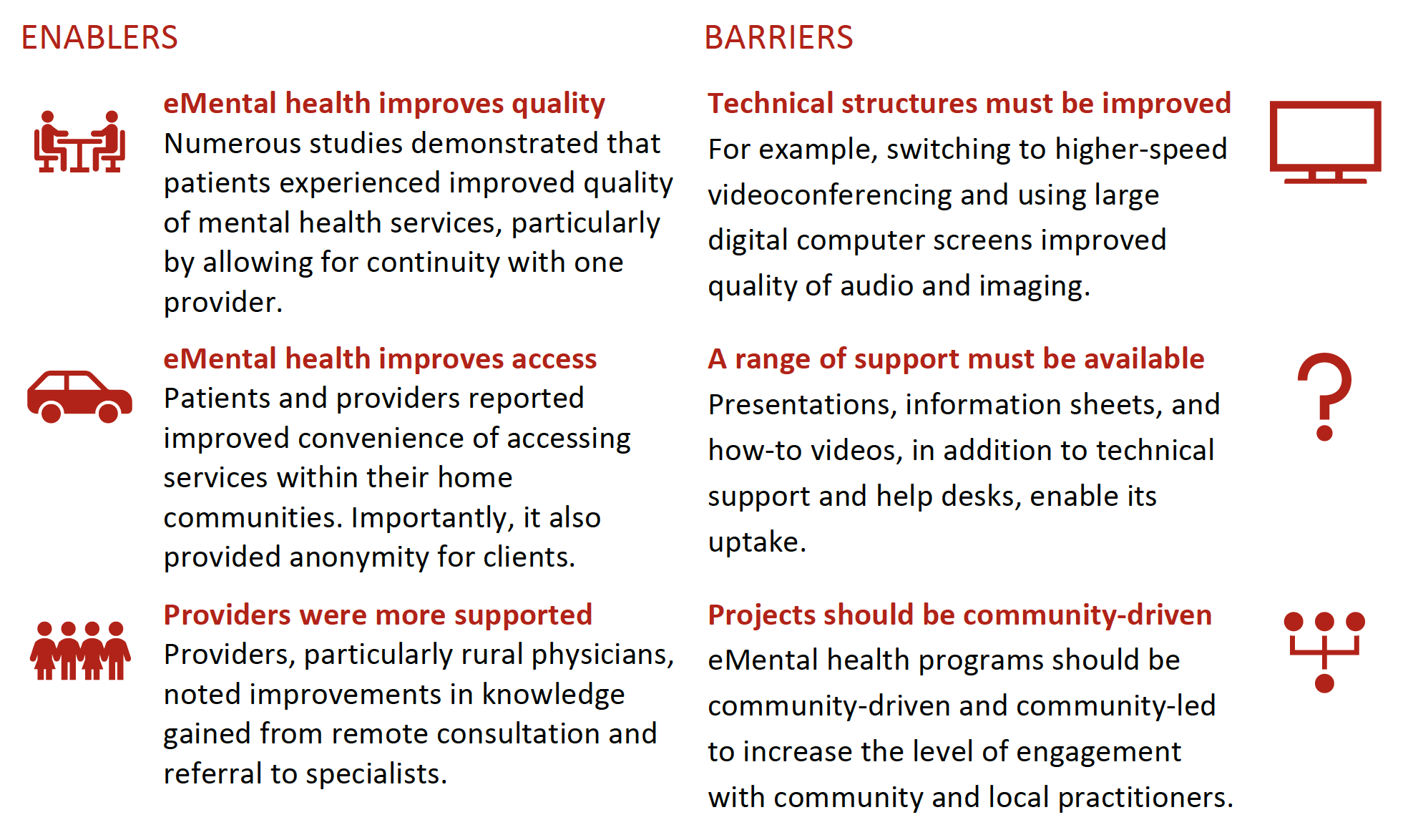
Rural patients and health care providers identify advantages and disadvantages in using eMental health. Health system users report increased access to care, decreased travel time, increased support, decreased hospital transfers, and stronger interpersonal relationships as advantages. Disadvantages include technical problems, privacy and confidentiality concerns, physical limitations, administrative difficulties, and inadequate health care provision.
Although patients and providers note these benefits or drawbacks based on their personal experiences, the success of an eMental health program may need to be reviewed on a larger scale. There is an association between modifiable systemic barriers and satisfaction levels, based on feedback from patients and providers. By focusing on the larger-scale enablers and barriers that underly the frustrations and successes that patients and providers experience using eMental health, disadvantages can be mitigated, and advantages can be amplified.

Primary systemic barriers to the success of telemedicine include inadequate technical equipment, funding/resource constraints, and resistance from health care providers, patients, and families. Enablers of the system include pre-established environment and care procedures, program promotion and training, regular contact among health care providers, technical improvements and support, organized administration, and planning procedures.
Technological issues often impede the successful uptake of eMental health in communities. Patients and providers report frustration with technology, including delayed speech and movement, sound echoes, and inadequate internet access. Rural areas that experience more technical problems report lower levels of utilization merely due to technological issues. If the infrastructure in which the technology operates is optimized, then the level of acceptance and integration of telemedicine into mental health services can be improved.