Report- Telepaediatrics in Rural and Remote Australia and Canada
Morris S, Steven S, LeBlanc M, Petrie S, Carson DB & PA Peters. (2019). Report: Telepaediatrics in rural and remote Australia and Canada. Spatial Determinants of Health Lab, Carleton University: Ottawa, ON. DOI: http://dx.doi.org/10.22215/sdhlab/2019.5
A high quality PDF of this report with references is available for download.
BACKGROUND
Rural and remote communities in Australia and Canada experience barriers to accessing healthcare services (1). These barriers are especially pronounced when attempting to access more specialized health care services, such as paediatric (2–4). Both countries have implemented programs that aim to bridge the gap between rural communities and specialized healthcare. One such service is telepaediatrics.
Telepaediatrics, as part of telehealth, refers to any paediatric health-related service, network, or medical tool that transmits voice, data, images and information through telecommunication programs as part of providing health services (5–7). Telehealth services are ideal because they remove the need to relocate the rural patient to urban specialist sites (5–7).
In a WHO survey (2010), 60% of member countries had telehealth services in place but only 30% of these programs were implemented as part of routine care (8). Only 3 member countries had established telepaediatric services in place (8). No previous investigations examine the use of telehealth programs in urban versus rural settings (8). This review aims to identify the common barriers to telepaediatric services in rural Australia and Canada and outlines suggestions for future implementation.
KEY FINDINGS

SOLUTIONS AND BARRIERS
This review identified 7 major barriers and 6 major solutions to establishing telepaediatric services in rural Australia and Canada, as outlined in the figure below. A major overall finding that facilitated the transition from barrier to solution was encouraging the continued cooperation between urban and rural healthcare settings. Given the lack of specialists in rural settings and the fact that urban specialists were often uninformed of the limitations in a rural healthcare setting (3,9–12), facilitating knowledge exchange between urban and rural practitioners was paramount to better serving patients and their families in ways that did not cause undue stress or hinder treatment plans.
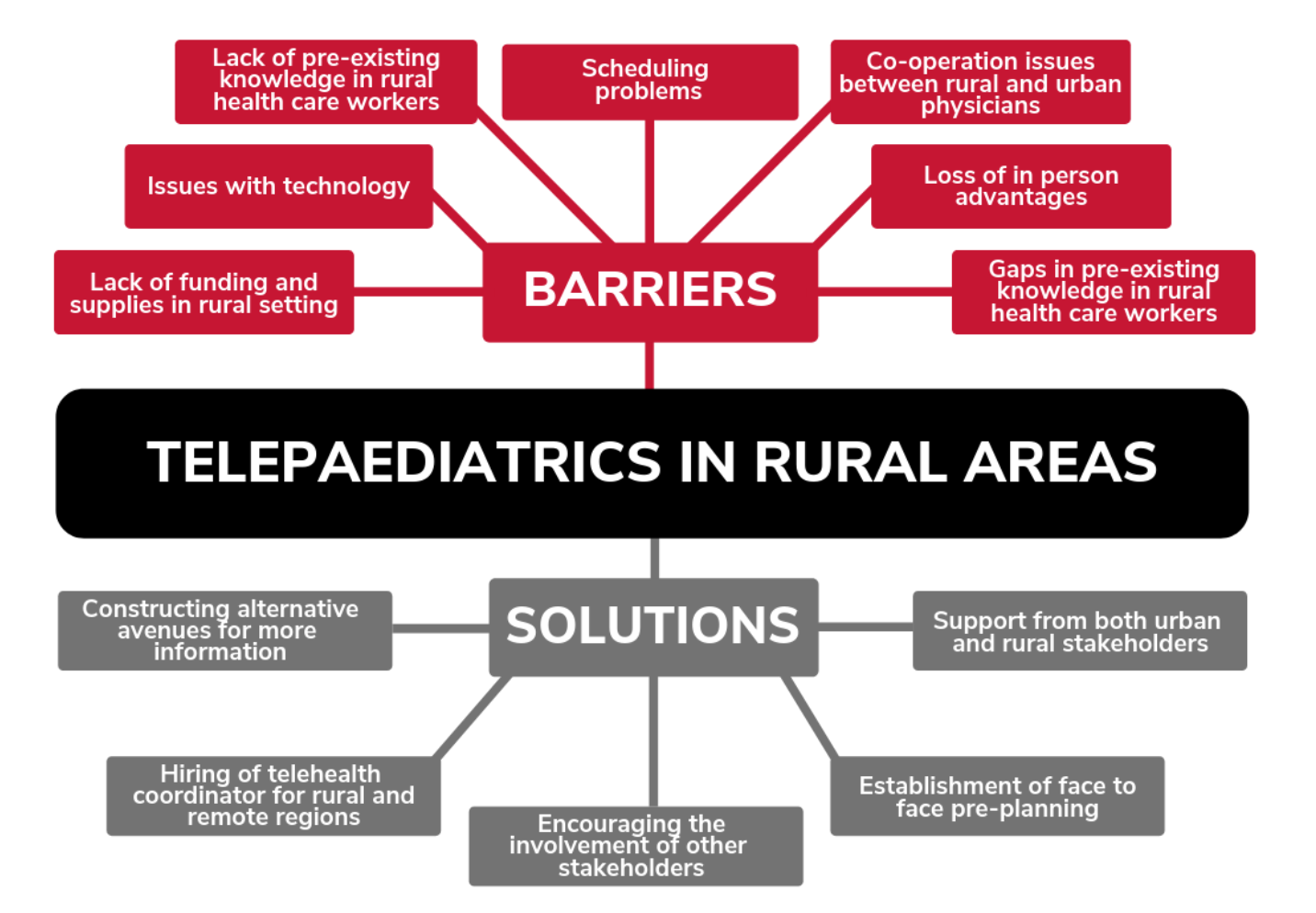
The single most reported solution across all literature was the need for a telehealth coordinator in rural and remote settings (3,9,11,13–19). This solution directly addresses the scheduling barrier (9,10,12,17,20,21) also identified in this review. Face to face pre-planning as a solution directly addressed the barrier that rural and urban physicians do not effectively co-operate in delivering telehealth (12). Patients reported that prior needs assessments with urban physicians were rarely conducted (3,10–12) and that a disagreement between urban and rural physicians over treatments, such as prescriptions, halted effective care (21). The solution of face to face pre-planning involving rural and urban physicians along with the patient and their family could effectively bridge this divide so interruptions to care do not occur.
FUTURE CONSIDERATIONS
Currently, no universal set of guidelines for establishing telepaediatric services exists in the literature. This review provides the beginning of a framework for building and implementing these services.
Considerations should be made surrounding rural specificity of healthcare (22). eHealth, a broad concept within which telehealth and thus telepaediatrics, falls as a framework for rural healthcare is still relatively new. Some rural and remote communities may have adopted these concepts more than others (23,24). Communities familiarity with this form of healthcare delivery should be taken into consideration in the method of implementation of the service and education of the community.
The use of telehealth is unable to completely outsource face-to-face meetings with health care professionals (10,11,15,19,25,26). It should not be expected that with the implementation of paediatric telehealth, any in-person contact with a specialized health care professional is dismissed. Face-to-face meetings are effective for establishing provider-patient trust and allows for more effective collaboration between the patient’s urban and rural physicians (6,27). This balance between when to use technology over face-to-face meetings, must be established in future telepaediatrics services in rural and remote areas.
Lastly, the uniqueness of paediatrics as a medical speciality, must be worked into the system of rural and remote telehealth services. For example, the child-friendliness of technology used in telepaediatrics, is much more important than the technology in telehealth approaches to other specialities (28,29). In addition, both the patient’s and caregiver’s reaction to telehealth practices and technology have to be accounted for, as one can influence the other and promote discontinuation of the service in some cases (15,30,31). Telehealth approaches to healthcare service delivery become especially important in a paediatric setting, where both children and caregiver would be need to relocated to urban specialist sites otherwise, increasing costs and induced stress (31,32).
METHODS
A structured scoping review was undertaken to identify and categorize literature regarding telepaediatric services, across various medical sub-specialties, in Australia and Canada. Searches were conducted in a general eHealth database created previously by two research reviewers. This review followed the framework proposed by Arksey & O’Malley (33). The five steps included in this framework were (1) identifying the research question (2) identifying relevant studies (3) study selection (4) charting the data (5) collating, summarizing and reporting the data. The scoping review identified 24 primary sourced articles that met inclusion criteria. Articles that were focused on the satisfaction, sustainability or effectiveness of the service delivery of the programs (i.e. if articles focused on economics or on technical functionality of the telehealth technology) were included.