Leblanc M, Petrie S, Carson DB, Paskaran S, & PA Peters. (2019) Patient and Provider Perspectives on Rural eHealth Interventions in Canada and Australia. Spatial Determinants of Health Lab, Carleton University: Ottawa, ON. DOI:10.22215/sdhlab/2019.3
A high-quality PDF of this report is available for download.
 Although health care is widely accessible in most developed countries, rural areas often struggle to adequately meet health care needs. Challenges in accessing and receiving adequate health care introduce large variations in disease levels, level of treatment, life expectancy, and overall health status for rural populations.
Although health care is widely accessible in most developed countries, rural areas often struggle to adequately meet health care needs. Challenges in accessing and receiving adequate health care introduce large variations in disease levels, level of treatment, life expectancy, and overall health status for rural populations.
eHealth, or electronic health, defined here as any electronic medium used to access health services, is a method used to bridge the gap between rural and urban centres to improve health care access. Including the above definition, eHealth also includes any technology designed to improve efficiencies and reduce costs in relation to health care. By providing a comprehensive overview of feedback from past interventions, policy-makers and program developers can develop strategies to improve the implementation and the use of eHealth technologies.
Although eHealth has been reported as a favourable method to increase access to health care, users report many disadvantages that warrant improvement. Updated technology, increased IT support and training, and regular meetings between urban and rural providers can improve the uptake of telemedicine in rural communities. Providers and stakeholders should recognize specific instances in which eHealth may not be the best option to deliver care, such as in mental health cases where face-to-face contact is important in treatment. The highly reported benefits of decreased travel, cost, and increased access to care indicate that the advantages of eHealth outweigh the disadvantages and will be an effective means to improve access to health care for rural areas.
Based on reviewed literature, eHealth is a favourable method to increase access to care, as denoted by levels of positive feedback from patients and providers. Although negative perspectives are still pervasive, effectively quantifying them is difficult.
| “It gives them access that other [patients] that are in more densely populated areas have and they don’t miss out because of their remote location.” |
The primary reported benefits of eHealth include decreased travel time, time/cost saving, and increased access to services, followed by effective technology, increased support, and increased patient involvement.
Decreased travel time was reported most from both patients and providers, regardless of the type of eHealth technology used. Before eHealth was introduced, travelling to and from appointments was an inconvenience; it took time away from work, from family, and from community involvement. The travel time and the travel itself can have negative effects on health, where patients can be exhausted from travel and may take longer to recover.
| “I didn’t have to travel, I didn’t have to give up a day’s work to take him somewhere and then have to worry about where I’m going to make that day’s wage up. I didn’t have to worry about what I was going to do with the other three kids, or do I pull the whole four of them out of school just to take one child to a therapist.” |
 eHealth allowed rural communities to access specialist services otherwise unavailable in the area, enabling health issues to be identified and addressed earlier. The use of technology has been shown repeatedly to save time and money, for both patients and for the health system. eHealth increased primary care levels and follow-up rates, which in turn reduced inappropriate referrals or transfers to urban centres. After using eHealth, rural health care providers reported an increased level of confidence and a broader skill set by observing specialists. Regular contact with specialists also allowed rural practitioners to seek help when necessary, decreasing isolation and creating a network of providers to provide support. In some instances, patients also felt more comfortable disclosing information through technology, which facilitated communication with providers.
eHealth allowed rural communities to access specialist services otherwise unavailable in the area, enabling health issues to be identified and addressed earlier. The use of technology has been shown repeatedly to save time and money, for both patients and for the health system. eHealth increased primary care levels and follow-up rates, which in turn reduced inappropriate referrals or transfers to urban centres. After using eHealth, rural health care providers reported an increased level of confidence and a broader skill set by observing specialists. Regular contact with specialists also allowed rural practitioners to seek help when necessary, decreasing isolation and creating a network of providers to provide support. In some instances, patients also felt more comfortable disclosing information through technology, which facilitated communication with providers.
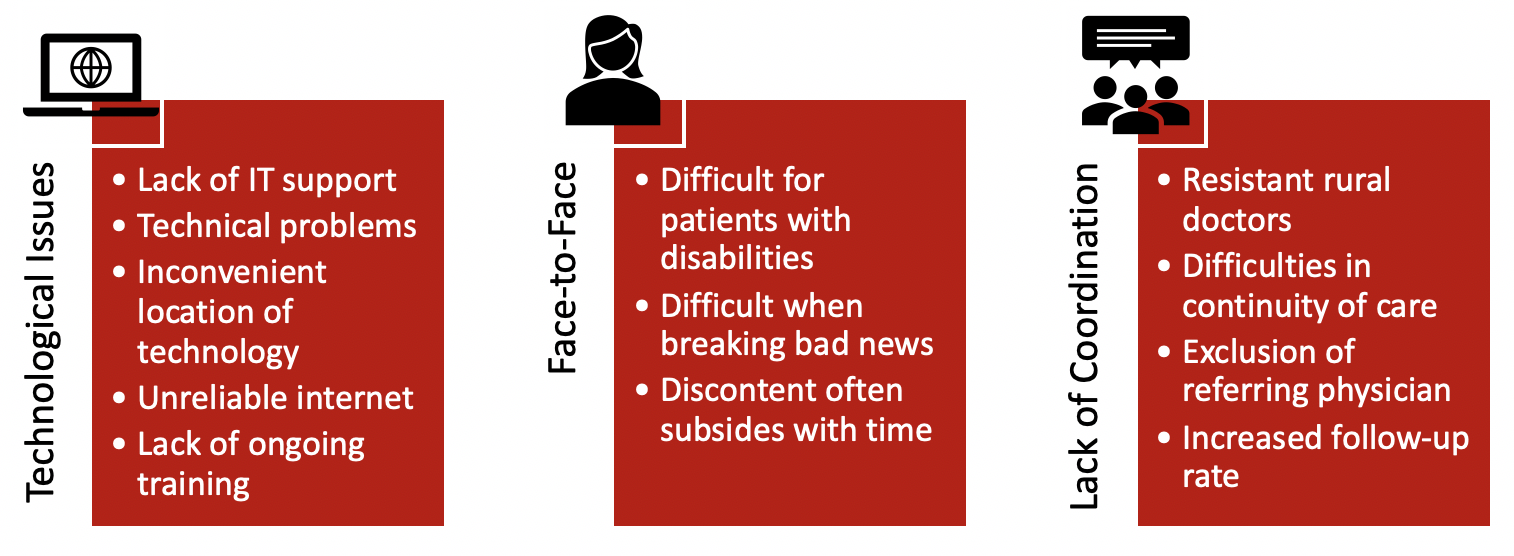
The primary disadvantages of telehealth identified were technological issues, lack of face-to-face contact, limited IT training, lack of coordination, confidentiality, and system cost. Technological issues stemmed from inadequate technology, such as insufficient broadband connection, and inadequate IT support or training.
Many successful programs implemented technology training programs and on-site IT support to facilitate the transition to eHealth for patients and providers. Preference for face-to-face contact varied among individuals, specialties, and situations. Providers identified specific instances in which it would not be appropriate to use eHealth, such as in feeding assessments in speech pathology. They also felt it was difficult to break bad news to patients using technology, or to note the subtle cues that could help form a more complete, accurate diagnosis. The importance of effective coordination between urban and rural providers introduced challenges, especially if the two physicians had differing opinions regarding treatment or delivery of care. The disagreements would confuse patients, leading to distrust of both providers. In some cases, the specialist was unaware of services or resources available in rural areas, which created unrealistic patient expectations. To facilitate communication, both providers should be available and easily contactable during consultations.