Report – Rural Physician Recruitment and Retention
Sendanyoye C, Sebastian S, Petrie S, Carson DB, & PA Peters. (2019) Report: Recruitment and retention of rural physicians. Spatial Determinants of Health Lab, Carleton University: Ottawa, ON. DOI:10.22215/sdhlab/2019.1
A high-quality PDF of this report is available for download.
Rural and remote communities comprise around 32% and 22% of Australia’s and Canada’s population. However, only 14% and 16% of family physicians in Australia and Canada, respectively, practice in these communities, resulting in a disproportion in access as compared with urban areas. An erosion of health services occurs when the number of physicians and other health care providers in a region is insufficient or these professionals are non-existent. Even when existing in a rural and remote region, providers are often overburdened. Inaccessibility to services in rural and remote communities’ results in poor health outcomes for all involved.
In Canada, 1 in 7 physicians will leave rural practice within two years. Strategies to address these turnover rates and the lessening interest in entering rural practice have focused on supporting recruitment and retention initiatives (RnR) to first bring physicians into rural practice and then encourage physicians to continue in rural practice beyond the short-term.
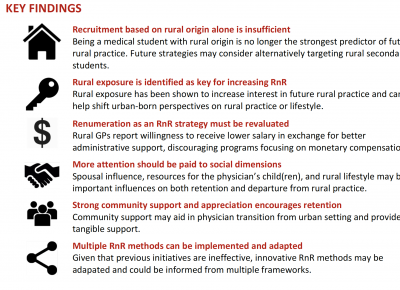
These programs have so far been insufficient or ineffective to address the lack of physicians in rural and remote areas. A review of recent literature related to RnR initiatives focused on rural physicians in Australia and Canada was conducted to investigate the strengths and limitations of initiatives. Further, this review critically examines the short and long-term feasibility of initiatives and develops a conceptual framework for designing or examining RnR initiatives.
Integrating Strategies
Given that many previous RnR initiatives follow similar strategies that are all largely unsuccessful, it is paramount that new methods of RnR for rural physicians are investigated and trialed. Findings in this review, such as the fact that renumeration must be re-evaluated, further emphasize the need to shift previous conceptualizations of RnR initiatives. Four main conceptual frameworks used in RnR initiatives for rural physicians were identified in this review.
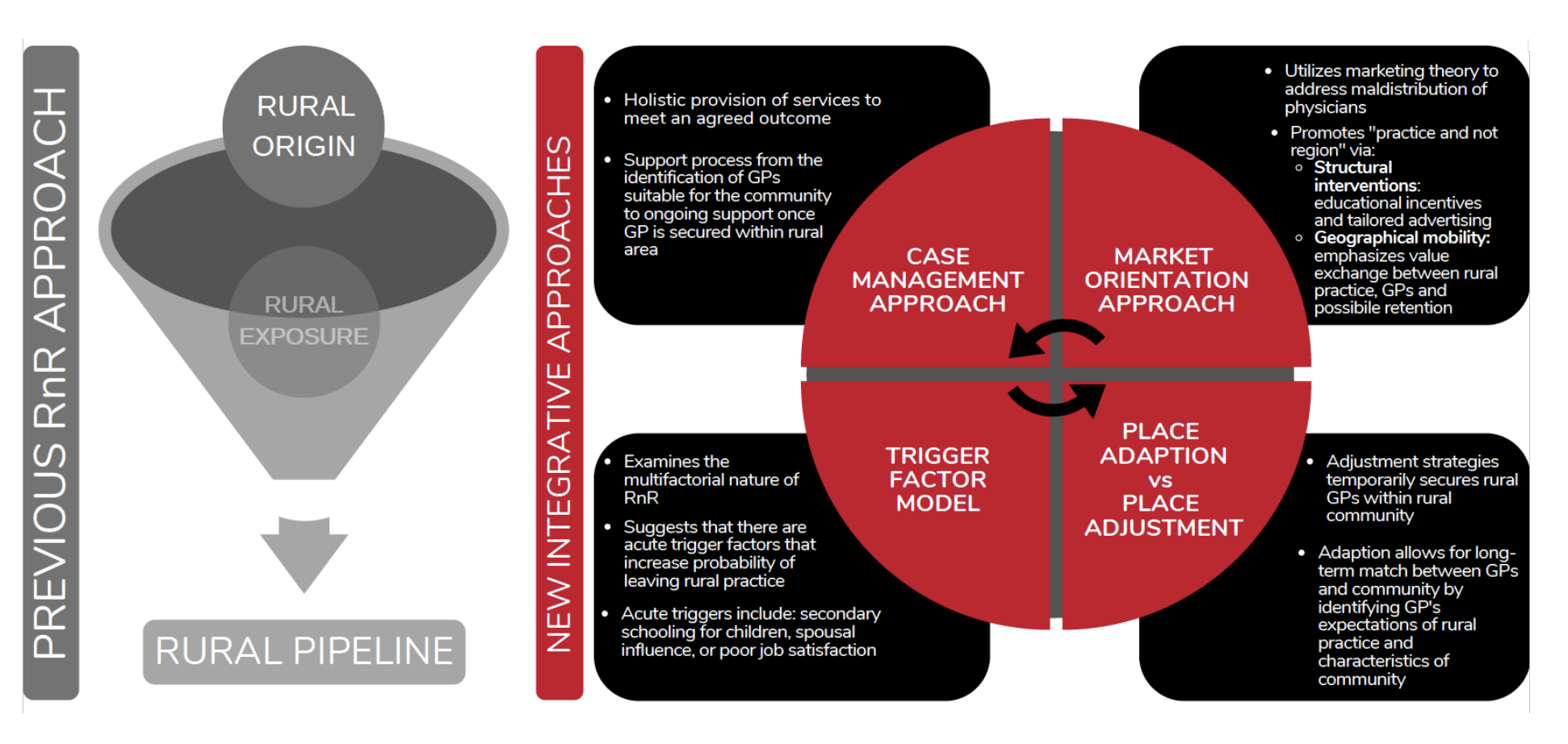
No conceptual RnR strategy identified in this review is superior to another, as each strategy encourages prioritization of different influences on bringing in and keeping physicians in rural communities. Rural and remote communities in Australia and Canada should be encouraged to consider their unique needs in order to select a model that fits best with satisfying those needs.
Communities should be empowered to select elements from various models that best fit the overall objective of community. Rural communities with characteristics of strong social support and high appreciation, mentioned previously as important retention factors for rural physicians in Australia and Canada, may select a marketing approach through a video that emphasizes these characteristics. Once a suitable physician has been recruited, the community may select elements from a case-management approach that focuses on addressing trigger factors with the physician, such as a concern of the lack of secondary schooling for their child in the new setting.
Future Directions
Progression towards effective, robust RnR of rural physicians requires embodying an interdisciplinary approach to studying these strategies, with a view towards later use by decision makers. Participatory Action Research could use extensive community surveillance and engagement to further identify factors that each community values. The findings from participatory action in these communities could then lead to more effective use of the Market Orientation Approach, in which more targeted initiatives can be created as informed by the community’s unique values. Additionally, findings from PAR may be able to inform the incoming physician and guide the next steps of determining the level of support needed from allied health professionals or the community at large.
The marketing approach and participatory action research combination may further benefit from Dirt Research, a form of ethnographic research in which findings are enhanced by engaging with community members in various social settings to understand the lived experience of these people. Dirt Research may provide the findings needed to incorporate the case management approach, so that additional needed training is provided and physician concerns in transition are addressed.
Lastly, effective knowledge translation that addresses the lack of physicians and ongoing RnR initiatives should be a point of emphasis in the future. Leveraging mentioned strategies through emphasizing emerging rural practice technologies (eHealth) and dispelling myths about rural living may result in more effective RnR and ultimately better health outcomes.
The complete PDF can be downloaded for citation.