Hondonga T, Sendanyoye C, Mahling A, Sourial M, Trto S, & PA Peters. (2021). “Report: Potential for eHealth in rural and remote follow-up care.” Spatial Determinants of Health Lab, Carleton University: Ottawa ON. DOI: 10.22215/sdhlab/2021.1.
A full PDF of this report is also available.
Rural and remote communities in Canada and Australia are disproportionally affected by barriers when accessing healthcare. Barriers include, but are not limited to: lengthy travel distances, inefficient communication between healthcare teams, and client disengagement in follow-up care (1–5). These barriers are notably evident when seeking access to more specialized health services (1). While, Canada and Australia have implemented electronic health (eHealth) technologies to mitigate issues of access to specialized healthcare services in rural and remote areas, their routine use in follow-up care has not been fully implemented (6,7).
 eHealth can be described as any technology that is used to deliver health services electronically (8). It is available in several mediums such as: mobile health, telehealth, and electronic health records. Mobile health is a medium in which healthcare services are delivered via mobile technologies such as smartphones, tablets, and wearables (9,10). Additionally, telehealth involves the use of telephones or video-conferencing technologies to correspond with clients, or remote client monitoring technologies to collect data on their clients’ health (6). Lastly, electronic health records are a form of eHealth technologies whereby health care providers securely store and share health information of clients (11,12).
eHealth can be described as any technology that is used to deliver health services electronically (8). It is available in several mediums such as: mobile health, telehealth, and electronic health records. Mobile health is a medium in which healthcare services are delivered via mobile technologies such as smartphones, tablets, and wearables (9,10). Additionally, telehealth involves the use of telephones or video-conferencing technologies to correspond with clients, or remote client monitoring technologies to collect data on their clients’ health (6). Lastly, electronic health records are a form of eHealth technologies whereby health care providers securely store and share health information of clients (11,12).
eHealth technologies have been promoted in rural and remote communities as they have demonstrated the potential to dissolve barriers of access to healthcare services, facilitate efficient health service delivery, improve client care, and health outcomes in hard-to-reach areas (13). However, further research into the advantages and disadvantages of eHealth services in rural and remote communities is warranted. Thus, this report aims to identify the advantages and disadvantages of eHealth services among service users in rural and remote communities in Australia and Canada; specifically, examining the role eHealth plays in follow-up care, client experiences using eHealth as an alternative to face-to-face appointments, and suggestions for future implementation.
KEY FINDINGS
ADVANTAGES AND DISADVANTAGES
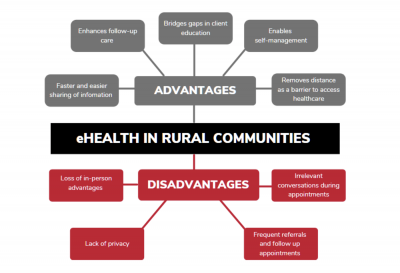
This review identified five advantages and four disadvantages of eHealth services for follow-up care for service users in rural and remote communities in Canada and Australia (Figure 1). eHealth services enabled healthcare team members to share information about diagnosis, test findings, imaging results, and medications with clients in a timely matter, avoiding unnecessary referrals and long-wait times for follow-up appointments (2,3,5). Consequently, physicians found eHealth facilitated improved client education and client self-management (2–5). eHealth services removed distance as a barrier to accessing health services. However, a major disadvantage of eHealth services included the inability to complete physical assessments (20,21). Moreover, clients reported a concerns about online privacy regarding the sharing of personal health information (14,16–19). Clients also felt that in some instances there was no need for follow-up appointments (16). Lastly, physicians reported non-relevant conversations took up extra time during appointments (16).
FUTURE CONSIDERATIONS
Although e-visits have proven to be beneficial in certain medical disciplines, in other fields they were deemed challenging (e.g., post-operative care). Therefore, it is imperative that future research analyzes how eHealth follow-up care can be implemented efficiently across various medical specialties. Logistical issues related to the availability of an electronic device and internet reliability remain common limitations. This issue may be addressed by an established eHealth site in a rural community, allowing e-visits for clients to save time and money on travel. Furthermore, alleviating client and provider privacy concerns is crucial for the sustainability of eHealth interventions. Promotion of secure and protected systems can offer clients reassurance on the safety and security of their private health information. In summary, a strong evidence-base is required centering these key priority areas to better inform policy and implementation of eHealth services in rural and remote communities.
METHODS
This report is based on a structured scoping review undertaken to identify the scope of research on the role eHealth plays in follow-up care in rural and remote regions of Canada and Australia. The identification of appropriate literature for this review followed Arksey and O’Malley’s five stage process, beginning with: 1) defining the key terms used in the search engines; 2) identification of relevant studies; 3) study selection based on a set of inclusion and exclusion criterion; 4) charting the data; and, 5) collating, summarizing, synthesizing and reporting on the findings of the articles (22). The scoping review identified 18 primary articles that met inclusion criteria. Articles focused on the role of eHealth, specifically barriers, enablers, and the utility of electronic health services in follow-up care.